Blocked tear ducts, also known as nasolacrimal duct obstruction, is a common pediatric eye condition in infants and young children.
While blocked tear ducts typically resolve on their own within the first year of life, many underlying causes can potentially be addressed by pediatricians, as well as several available treatment options for both parents and caregivers.
What Are Blocked Tear Ducts?
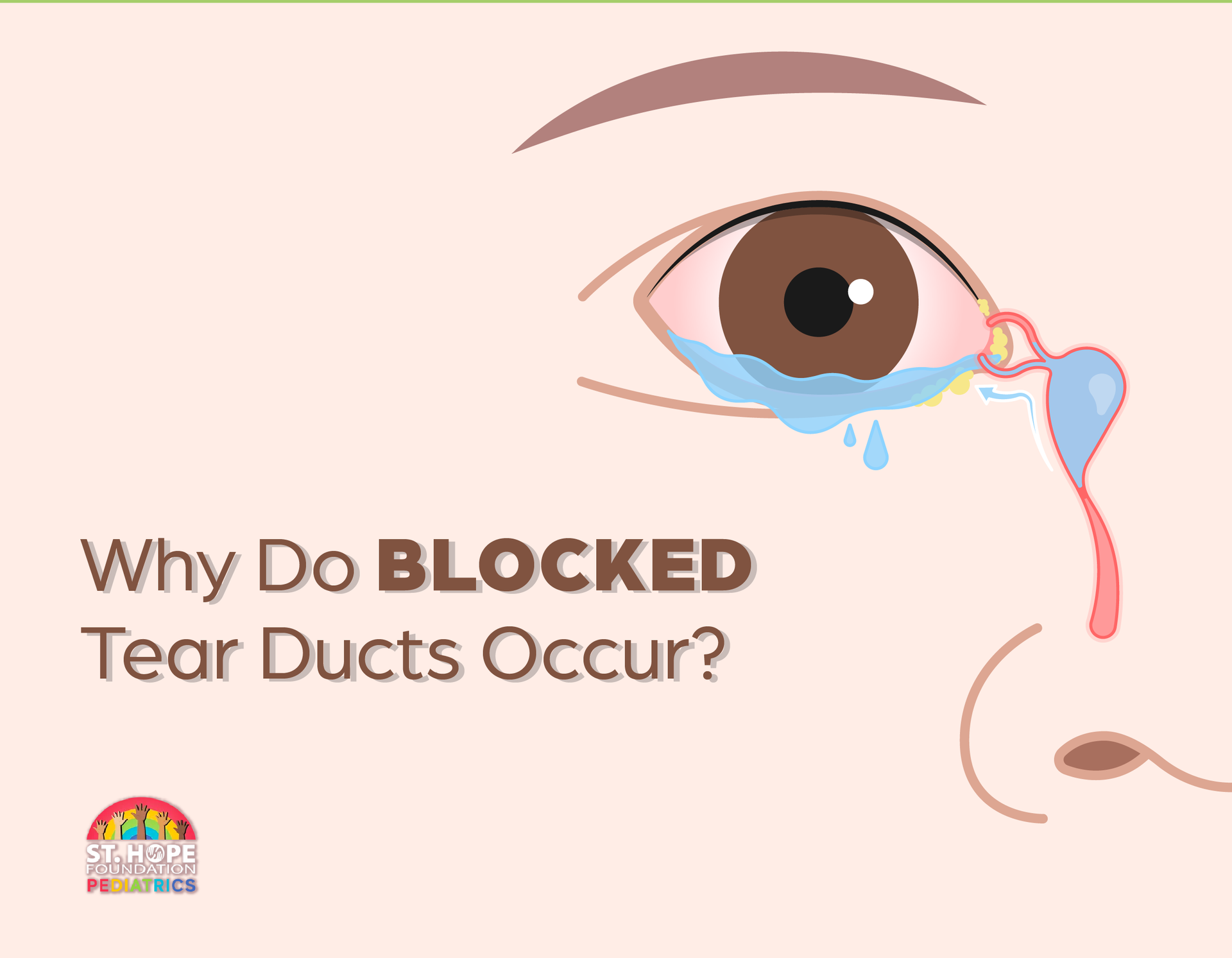
The tear ducts, or nasolacrimal ducts, are narrow channels that drain tears from the eyes into the nasal cavity. When these ducts become blocked or obstructed, tears are unable to drain properly, leading to symptoms such as excessive tearing, eye discharge and potential eye infections.
Blocked tear ducts are relatively common in newborns and infants, affecting approximately 5 to 20 percent of newborns.
Causes of Blocked Tear Ducts in Children
Several factors can contribute to the development of blocked tear ducts in children, including:
- Congenital Anomalies:
In some cases, blocked tear ducts occur due to congenital abnormalities or malformations of the nasolacrimal duct system. Structural abnormalities, such as narrow or underdeveloped tear ducts, can impede the normal drainage of tears, leading to obstruction.
- Membranous Blockages: Blockages within the tear ducts can also occur due to the presence of membranous obstructions or tissue growths that obstruct the flow of tears. These blockages may be present from birth or develop later in infancy.
- Inflammation or Infection:
Inflammatory conditions, such as dacryocystitis (inflammation of the tear sac) or conjunctivitis (pink eye), can cause swelling and inflammation of the tear ducts, leading to obstruction. Bacterial or viral infections can also contribute to the development of blocked tear ducts in children.
- Nasal Bone Compression:
During childbirth, pressure on the infant's nasal bones can sometimes result in temporary compression or deformation of the nasolacrimal ducts, leading to transient blockages. While these blockages often resolve spontaneously, they can contribute to symptoms of tearing and eye discharge in newborns.
- Delayed Tear Duct Development: In some cases, blocked tear ducts may occur due to delayed development or maturation of the tear duct system in newborns. As the tear ducts continue to develop and open over time, symptoms of tearing and eye discharge may gradually improve.
Risk Factors for Blocked Tear Ducts
Several factors may increase a child's risk of developing blocked tear ducts, including:
- Premature birth or low birth weight
- Family history of tear duct abnormalities
- History of nasal or sinus infections
- Anatomical abnormalities of the face or nasal passages
- Exposure to environmental irritants or pollutants
It's essential for parents and caregivers to be aware of these risk factors and monitor their child's eye health closely for any signs of blocked tear ducts.
Treatment Options for Blocked Tear Ducts
In most cases, blocked tear ducts in children will resolve spontaneously within the first year of life without the need for intervention. However, if symptoms persist or complications arise, pediatricians and eye care professionals may recommend the following treatment options:
- Massage Therapy: Gentle massage techniques applied to the tear duct area can help promote tear drainage and alleviate symptoms of tearing and eye discharge. Parents can perform massage therapy at home under the guidance of a healthcare provider.
- Warm Compresses: Applying warm compresses to the affected eye can help soothe inflammation, reduce swelling and facilitate the clearance of blockages within the tear ducts. Warm compress therapy can be performed several times a day as needed.
- Antibiotic Eye Drops: In cases where blocked tear ducts are associated with bacterial infections or inflammation, pediatric eye care professionals may prescribe antibiotic eye drops to reduce infection and promote healing.
- Tear Duct Probing and Irrigation:
If conservative measures fail to resolve the blockage, pediatric ophthalmologists may recommend tear duct probing and irrigation procedures to clear obstructions and restore normal tear drainage. These minimally invasive procedures are typically performed under sedation or general anesthesia in a clinical setting.
- Silicone Tube Placement: In cases of persistent or recurrent tear duct obstruction, silicone tube placement may be necessary. This involves silicone tubes being inserted into the tear ducts to keep them open and allow tears to drain properly.
Get Treatment for Your Child’s Blocked Tear Ducts at St. Hope Pediatrics
Take the first step towards improving your child's eye health by scheduling an appointment with St. Hope Pediatrics today. Our experienced team of pediatric specialists is dedicated to providing compassionate care and effective treatments for conditions like blocked tear ducts.
Contact us here on our website or give us a call at (713) 778-1300.